When my grandmother turned 82, I noticed something that worried me deeply. The woman who once prepared elaborate Sunday roasts and baked fresh bread weekly was now struggling to cook even simple meals. Her appetite had diminished, and she’d lost nearly 15 pounds in just three months. That’s when her doctor suggested something I hadn’t considered: meal replacement shakes.
This conversation sparked my deep dive into understanding the pros and cons of meal replacement shakes for elderly individuals. What I discovered was far more nuanced than I expected—these convenient nutritional solutions can be lifesaving for some seniors while potentially problematic for others.
If you’re caring for an aging parent, grandparent, or are a senior yourself wondering whether meal replacement shakes are right for you, you’re in the right place. Let’s explore this topic together with honesty, compassion, and evidence-based insights. 🥤
Key Takeaways
- Meal replacement shakes can provide complete nutrition when whole food consumption becomes difficult due to appetite loss, swallowing difficulties, or mobility limitations
- Convenience is a major benefit for elderly individuals who struggle with meal preparation, but shouldn’t completely replace the social and sensory experience of eating whole foods
- Cost considerations matter—quality meal replacement shakes can be expensive, ranging from $2-$8 per serving, which adds up quickly on fixed retirement incomes
- Not all shakes are created equal—some contain high sugar levels and artificial ingredients that may not suit specific health conditions like diabetes or kidney disease
- Professional guidance is essential—consulting with a geriatric nutritionist ensures meal replacement shakes complement rather than compromise overall health
Understanding Meal Replacement Shakes for Seniors

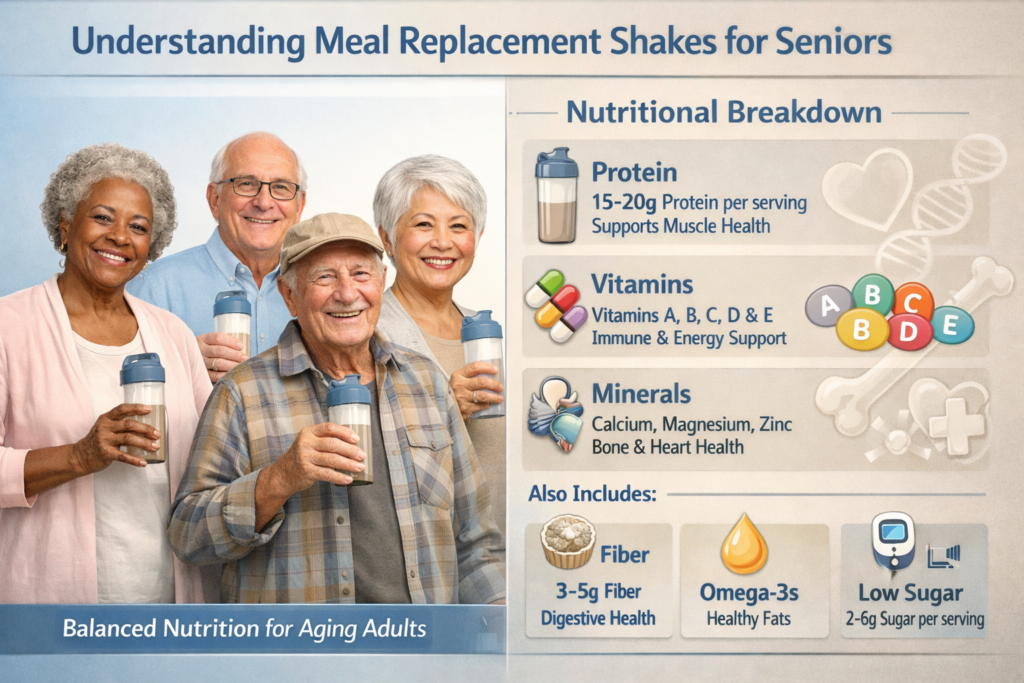
Before we dive into the advantages and disadvantages, let’s establish what we’re actually talking about. Meal replacement shakes are beverages designed to provide a nutritionally complete meal in liquid form. They typically contain a balanced mix of proteins, carbohydrates, fats, vitamins, and minerals.
For elderly individuals, these products come in several forms:
- Ready-to-drink bottles (most convenient)
- Powder formulas (requiring mixing with water or milk)
- Specialized medical nutrition products (prescribed for specific conditions)
- Standard commercial shakes (available at supermarkets and pharmacies)
Why Are Seniors Turning to Meal Replacement Shakes?
The aging process brings unique nutritional challenges. I’ve seen this firsthand not just with my grandmother, but through conversations with dozens of families navigating similar situations.
Common reasons elderly individuals consider meal replacement shakes include:
- Decreased appetite due to medication side effects or natural aging changes
- Difficulty chewing or swallowing (dysphagia)
- Limited mobility making meal preparation challenging
- Living alone and lacking motivation to cook for one person
- Cognitive decline affecting ability to plan and prepare meals
- Recovery from illness or surgery requiring increased nutrition
- Unintentional weight loss that concerns healthcare providers
According to recent Australian health data, approximately 30-40% of community-dwelling elderly adults are at risk of malnutrition, with rates climbing to 50-60% among those in residential care facilities [1]. This sobering statistic highlights why convenient nutritional solutions have become increasingly important.
The Advantages: Pros of Meal Replacement Shakes for Elderly
Let me share what I learned about the genuine benefits these products can offer. When my grandmother started incorporating meal replacement shakes into her routine, I witnessed several positive changes that surprised me.
1. Complete Nutritional Profile in Every Serving 🍎
One of the most compelling advantages is the guaranteed nutritional content. Quality meal replacement shakes are formulated to provide:
- 20-30 grams of protein per serving (crucial for maintaining muscle mass)
- Essential vitamins and minerals at levels meeting daily requirements
- Balanced macronutrients with appropriate calorie density
- Fiber for digestive health
- Fortified nutrients specifically beneficial for aging bodies
When my grandmother was barely eating half a sandwich for lunch, at least I knew her afternoon shake was delivering complete nutrition. This peace of mind was invaluable for our family.
2. Easier to Consume Than Solid Foods
For seniors experiencing dysphagia (swallowing difficulties), meal replacement shakes can be genuinely lifesaving. The smooth, liquid consistency:
- Reduces choking risk compared to solid foods
- Requires less chewing effort for those with dental issues
- Goes down more easily when appetite is suppressed
- Can be consumed slowly over time without food spoiling
I remember watching my grandmother struggle through a plate of food that would take her 45 minutes to finish. With shakes, she could sip throughout the morning without pressure or discomfort.
3. Tremendous Convenience and Time-Saving ⏰
Let’s be honest—convenience matters, especially for elderly individuals managing multiple health conditions or mobility limitations. Meal replacement shakes offer:
- No cooking required (particularly important for those with cognitive decline or safety concerns around stoves)
- Minimal cleanup (just rinse a glass or dispose of a bottle)
- Portable nutrition (easy to consume anywhere, even in bed if needed)
- Long shelf life (reducing shopping frequency)
- Consistent preparation (no recipe following or decision-making fatigue)
For seniors living in retirement communities or those who’ve lost a spouse and find cooking for one person depressing, this convenience can be transformative.
4. Precise Portion Control and Calorie Management
Many elderly individuals struggle with either under-eating or over-eating. Meal replacement shakes provide:
- Exact calorie counts (typically 200-400 calories per serving)
- Consistent portions (removing guesswork)
- Easy tracking for healthcare providers monitoring nutritional intake
- Controlled serving sizes that prevent overwhelming portions
This precision is particularly valuable when working with healthcare teams to address weight loss or gain goals.
5. Enhanced Appetite Stimulation
Interestingly, I discovered that some seniors find starting the day with a shake actually improves their appetite for later meals. The nutritional boost can:
- Provide energy that increases interest in food
- Establish a routine that encourages regular eating patterns
- Prevent the weakness that further suppresses appetite
- Serve as a bridge to more substantial meals
My grandmother found that having a shake at breakfast made her more interested in a proper lunch—something we hadn’t anticipated.
6. Cost-Effective Compared to Wasted Food
While individual shakes can seem expensive, consider this perspective: How much food gets thrown away when an elderly person can’t finish meals or forgets about groceries spoiling in the fridge?
For some families, meal replacement shakes actually reduce overall food costs by:
- Eliminating waste from uneaten prepared meals
- Reducing grocery shopping frequency and impulse purchases
- Preventing spoilage of perishable ingredients
- Providing predictable budgeting for nutritional needs
7. Medical-Grade Options for Specific Conditions
Specialized meal replacement shakes exist for virtually every health condition common in elderly populations:
| Condition | Specialized Formula Features |
|---|---|
| Diabetes | Low glycemic index, controlled carbohydrates, high fiber |
| Kidney Disease | Reduced protein, controlled potassium and phosphorus |
| Heart Disease | Low sodium, heart-healthy fats, plant sterols |
| Cancer Recovery | High calorie density, elevated protein, immune support |
| Digestive Issues | Pre-digested proteins, easily absorbed nutrients |
These targeted formulations can be incredibly valuable when managed properly with healthcare guidance. Understanding why protein supplements are important for elderly patients can help you make informed decisions about specialized formulas.
8. Social and Emotional Benefits
This might surprise you, but I’ve heard from several seniors who found meal replacement shakes reduced mealtime stress and anxiety:
- No pressure to finish a full plate of food
- Reduced embarrassment about eating slowly or messily
- Easier to consume discreetly when self-conscious about eating difficulties
- Less worry about cooking safety for those with memory issues
The Disadvantages: Cons of Meal Replacement Shakes for Elderly
Now let’s discuss the other side of the equation. As beneficial as these products can be, they’re not without significant drawbacks. Understanding these limitations is crucial for making informed decisions.
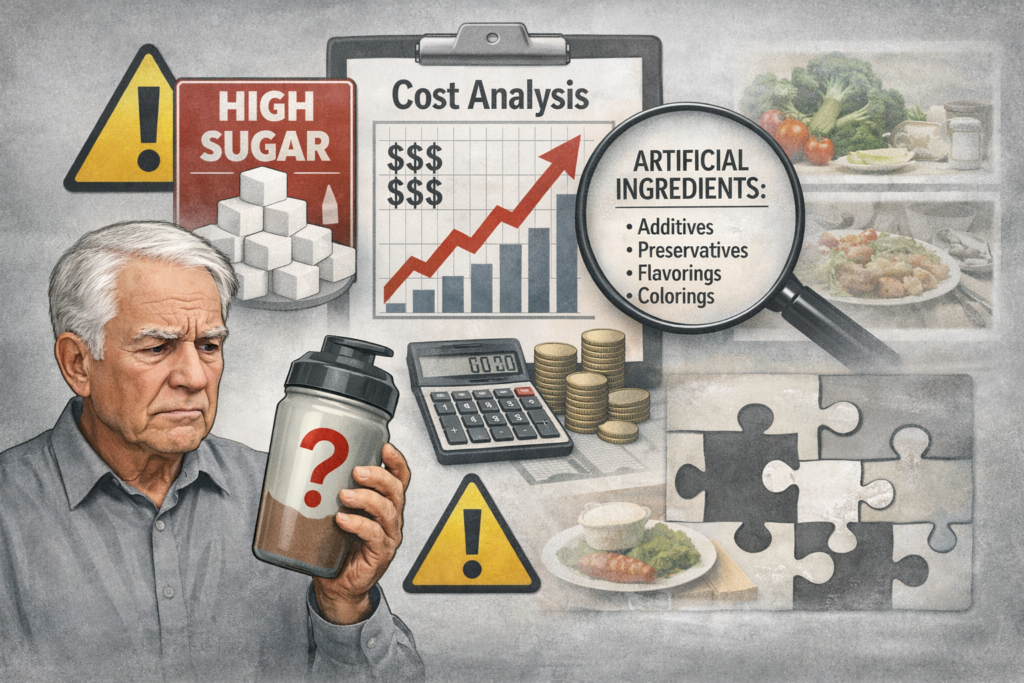
1. High Cost Can Strain Fixed Incomes 💰
Let’s talk numbers. Quality meal replacement shakes typically cost:
- $2-$4 per serving for standard commercial brands
- $4-$8 per serving for medical-grade specialized formulas
- $60-$240+ per month if replacing one meal daily
- $180-$720+ per month if replacing multiple meals daily
For seniors on fixed retirement incomes, this expense can be prohibitive. I watched my grandmother’s face when we calculated that replacing just her breakfast and lunch would cost nearly $300 monthly—more than her entire previous grocery budget.
Some families face difficult choices between nutritional supplements and other essential expenses like medications or utilities.
2. Missing the Joy and Social Aspects of Eating 🍽️
This is perhaps the most overlooked disadvantage. Eating is fundamentally social and cultural. When meal replacement shakes become the primary nutrition source, seniors may lose:
- Social connection during shared family meals
- Cultural food traditions that provide identity and comfort
- Sensory pleasure from diverse tastes, textures, and aromas
- Routine structure that mealtimes provide to the day
- Cognitive stimulation from meal planning and preparation
I noticed my grandmother became somewhat isolated when she relied heavily on shakes. She’d skip family dinners because “I already had my shake,” missing the conversation and connection that mattered more than the food itself.
3. Potential for Nutritional Gaps Despite “Complete” Formulas
While marketed as nutritionally complete, meal replacement shakes may not provide:
- Phytonutrients and antioxidants found abundantly in whole foods
- Beneficial fiber diversity (they contain fiber, but not the variety from different food sources)
- Bioavailable nutrients in the same form as whole foods
- Probiotic benefits from fermented foods
- Hydration from water-rich whole foods like fruits and vegetables
Emerging research suggests that whole food matrices provide nutritional benefits that isolated nutrients in shakes cannot fully replicate [2].
4. High Sugar Content in Many Commercial Brands 🍬
This shocked me when I started reading labels carefully. Many popular meal replacement shakes contain:
- 15-25 grams of sugar per serving (equivalent to 4-6 teaspoons)
- High glycemic loads that spike blood sugar
- Artificial sweeteners in “sugar-free” versions (with controversial health effects)
- Hidden sugars listed under various names (maltodextrin, corn syrup solids, etc.)
For elderly individuals with diabetes or pre-diabetes (affecting over 30% of Australian seniors), this sugar content can be genuinely problematic. Always check with healthcare providers, particularly when considering nutritional drinks for elderly health.
5. Digestive Issues and Intolerance
Not everyone tolerates meal replacement shakes well. Common complaints include:
- Bloating and gas (especially from high fiber content or sugar alcohols)
- Diarrhea or constipation (depending on formula and individual digestion)
- Lactose intolerance symptoms (many shakes contain dairy)
- Nausea (particularly when consumed too quickly or on an empty stomach)
- Artificial taste that some find unpalatable
My grandmother experienced significant bloating with her first brand and had to try three different products before finding one her system tolerated.
6. Risk of Over-Reliance and Reduced Food Variety
Perhaps the most insidious disadvantage is how convenient solutions can become complete replacements rather than supplements. This leads to:
- Decreased motivation to prepare or eat whole foods
- Loss of cooking skills and confidence
- Reduced dietary variety over time
- Muscle atrophy in chewing and swallowing if not regularly exercised
- Psychological dependence on the convenience
Healthcare professionals emphasize that meal replacement shakes should supplement, not substitute a varied diet whenever possible.
7. Artificial Ingredients and Additives
Many commercial meal replacement shakes contain:
- Artificial flavors and colors
- Preservatives for extended shelf life
- Emulsifiers and stabilizers (like carrageenan, which some research links to digestive inflammation)
- Synthetic vitamins and minerals (potentially less bioavailable than food-derived nutrients)
- Processed protein sources (like protein isolates rather than whole food proteins)
While generally recognized as safe, some elderly individuals prefer more natural options or have sensitivities to these additives.
8. Inadequate Hydration
This is subtle but important. When seniors replace meals with shakes, they may miss the hydration from water-rich whole foods like:
- Fresh fruits (watermelon, oranges, berries)
- Vegetables (cucumbers, tomatoes, lettuce)
- Soups and broths
- Yogurt and cottage cheese
Dehydration is already a significant risk for elderly individuals, and relying heavily on shakes without compensating with additional water intake can worsen this issue [3].
9. Potential Drug-Nutrient Interactions ⚠️
Meal replacement shakes’ concentrated vitamin and mineral content can interact with common medications:
- Vitamin K in shakes may interfere with blood thinners like warfarin
- High calcium content can reduce absorption of certain antibiotics and thyroid medications
- Iron fortification may interact with medications for Parkinson’s disease
- Potassium levels matter for those on certain blood pressure medications
This is why professional guidance from a geriatric nutritionist is so valuable—they can identify potential interactions your general practitioner might miss.
Finding the Right Balance: When Are Meal Replacement Shakes Appropriate?
After exploring both sides thoroughly, you might be wondering: “So should my elderly loved one use meal replacement shakes or not?”
The answer, as with most things in healthcare, is: it depends.
Ideal Scenarios for Meal Replacement Shake Use
Meal replacement shakes are most beneficial when:
✅ Recovering from illness or surgery requiring increased nutrition
✅ Experiencing unintentional weight loss despite efforts to eat more
✅ Dealing with dysphagia or severe chewing difficulties
✅ Supplementing (not replacing) inadequate whole food intake
✅ Managing specific medical conditions with appropriate specialized formulas
✅ Providing convenient nutrition during travel or busy periods
✅ Used as snacks between meals rather than meal replacements
Situations Requiring Caution or Alternatives
Meal replacement shakes may not be appropriate when:
❌ The elderly person can eat whole foods adequately (shakes aren’t necessary)
❌ Cost creates financial hardship (explore more affordable nutritional strategies)
❌ Digestive intolerance persists despite trying multiple brands
❌ Social isolation increases due to skipping shared meals
❌ They become the sole nutrition source without medical supervision
❌ Underlying appetite issues haven’t been medically evaluated
Practical Tips for Using Meal Replacement Shakes Wisely
If you decide meal replacement shakes are appropriate, here are strategies I’ve learned for maximizing benefits while minimizing drawbacks:
Choosing Quality Products 🔍
Look for shakes that provide:
- At least 15-20g protein per serving
- Less than 10g added sugar (or appropriate for medical condition)
- Minimal artificial ingredients
- Appropriate calorie density (250-400 calories for meal replacement)
- Third-party quality testing certifications
Avoid products with:
- Sugar as the first or second ingredient
- Long lists of unpronounceable additives
- Unrealistic health claims
- Inadequate protein content (less than 10g)
Integration Strategies
Best practices include:
- Use as supplements, not replacements whenever possible
- Maintain at least one whole food meal daily for social connection and dietary variety
- Rotate different flavors and brands to prevent taste fatigue
- Enhance with whole food additions (blend in fresh fruit, nut butter, or vegetables)
- Establish a consistent routine (same time daily helps with adherence)
- Monitor and adjust based on weight, energy levels, and overall wellbeing
Making Shakes More Palatable
Many seniors find commercial shakes too sweet or artificial-tasting. Try:
- Serving chilled or over ice (temperature can improve palatability)
- Adding coffee or tea for familiar flavors
- Mixing with whole milk instead of water for richer taste and extra calories
- Blending with frozen fruit for smoothie-like texture
- Using a straw (can make consumption easier and more pleasant)
- Trying different brands until finding preferred flavors
Cost-Saving Strategies 💡
To reduce the financial burden:
- Buy in bulk when possible (significant per-serving savings)
- Compare unit prices across brands and retailers
- Ask about medical necessity (some specialized formulas may be partially covered by insurance or subsidized)
- Consider homemade alternatives (whole food smoothies with protein powder can be more affordable)
- Look for sales and coupons (many manufacturers offer first-time customer discounts)
- Join senior discount programs at pharmacies and nutrition stores
Alternatives and Complementary Approaches
Meal replacement shakes aren’t the only solution for elderly nutritional challenges. Consider these alternatives or complementary strategies:
Whole Food Smoothies
Homemade smoothies using whole ingredients offer:
- Greater control over sugar content
- Fresh, natural ingredients
- Cost savings
- Customizable nutrition
- Similar convenience to commercial shakes
Basic elderly-friendly smoothie formula:
- 1 cup liquid (milk, yogurt, or fortified plant milk)
- 1 cup fruit (fresh or frozen)
- 1 scoop protein powder
- 1 tablespoon healthy fat (nut butter, avocado, or ground flaxseed)
- Optional: handful of spinach or kale (surprisingly undetectable in flavor)
Nutrient-Dense Snacks
Instead of full meal replacements, focus on nutrient-dense snacks throughout the day:
- Greek yogurt with honey and nuts
- Cheese and whole grain crackers
- Hard-boiled eggs
- Nut butter on apple slices
- Trail mix with dried fruit
- Hummus with vegetables
Meal Delivery Services
For seniors struggling with meal preparation but able to eat whole foods, meal delivery services designed for elderly individuals offer:
- Pre-portioned ingredients or fully prepared meals
- Nutritionally balanced options
- Variety and whole food benefits
- Social aspect of “real” meals
- Often comparable cost to quality meal replacement shakes
Community Resources
Don’t overlook community support options:
- Meals on Wheels programs
- Senior center lunch programs
- Church or community group meal sharing
- Volunteer shopping assistance
- Cooking classes specifically for seniors
For seniors looking to stay engaged and connected, exploring things to do in retirement can help maintain social connections that naturally include shared meals.
Working with Healthcare Professionals
I cannot stress this enough: professional guidance is essential when making significant changes to an elderly person’s nutrition.
When to Consult Healthcare Providers
Seek professional advice before starting meal replacement shakes if:
- The elderly person has multiple chronic conditions
- They take multiple medications
- Unintentional weight loss exceeds 5% of body weight
- Swallowing difficulties have developed
- Appetite changes are sudden or severe
- Cognitive decline affects eating ability
Questions to Ask Your Healthcare Team
When discussing meal replacement shakes with doctors or nutritionists, ask:
- “Are meal replacement shakes appropriate for this specific situation?”
- “Which brands or formulas do you recommend given current medications and conditions?”
- “How many servings per day are appropriate?”
- “What whole foods should still be prioritized?”
- “What warning signs should we watch for?”
- “How often should nutritional status be reassessed?”
- “Are there any specific nutrients we should supplement separately?”
The Value of Geriatric Nutritionists
A geriatric nutritionist specializes in the unique nutritional needs of aging bodies and can:
- Conduct comprehensive nutritional assessments
- Create personalized meal plans balancing shakes and whole foods
- Monitor for drug-nutrient interactions
- Adjust recommendations as health status changes
- Provide family education and support
- Connect you with community resources
The investment in professional nutritional guidance often pays for itself through improved health outcomes and reduced hospitalizations.
Real Stories: Learning from Others’ Experiences
Throughout my research and personal experience, I’ve encountered numerous families navigating this decision. Let me share a few stories that illustrate the complexity of this issue.
Margaret’s Story: The Right Tool at the Right Time
Margaret, 78, suffered a stroke that affected her swallowing ability. For three months during recovery, meal replacement shakes were literally lifesaving—they prevented malnutrition while she worked with speech therapists to regain swallowing function.
Once her swallowing improved, her family gradually reintroduced whole foods while maintaining one shake daily as a nutritional safety net. Two years later, Margaret eats normally but keeps meal replacement shakes on hand for days when she’s too tired to cook.
The lesson: Meal replacement shakes served their purpose during acute need, then transitioned to a supplemental role.
Robert’s Story: When Convenience Became Isolation
Robert, 81, discovered meal replacement shakes after his wife passed away. The convenience was initially appealing—no cooking, no cleanup, no reminders of eating alone.
Within six months, Robert had almost completely stopped preparing food. He’d declined several family dinner invitations because “I’ve already had my shakes.” His daughter noticed he seemed increasingly depressed and isolated.
With encouragement, Robert joined a senior center lunch program three times weekly and reserved shakes for breakfast only. The social interaction during shared meals significantly improved his mood and overall wellbeing.
The lesson: Convenience shouldn’t come at the cost of social connection and quality of life.
Linda’s Story: Finding the Right Balance
Linda, 73, has diabetes and early-stage kidney disease. Her nephrologist recommended specialized meal replacement shakes to ensure adequate nutrition while controlling protein, potassium, and phosphorus levels.
Linda uses one specialized shake daily for lunch (her least favorite meal to prepare) but prioritizes cooking dinner—her favorite activity and creative outlet. This balance provides medical benefit while maintaining her sense of independence and enjoyment.
The lesson: Meal replacement shakes can be part of a comprehensive strategy that respects both medical needs and personal preferences.
Making Your Decision: A Framework for Families
If you’re trying to decide whether meal replacement shakes are right for your situation, work through this decision-making framework:
Step 1: Assess the Current Situation
Honestly evaluate:
- Is adequate nutrition being achieved with current eating patterns?
- What specific challenges exist (appetite, preparation, swallowing, etc.)?
- What are the consequences of not addressing nutritional inadequacy?
- What resources (financial, social, medical) are available?
Step 2: Explore All Options
Consider:
- Can whole food approaches address the challenges?
- Are community resources available?
- Would meal delivery services be appropriate?
- Are meal replacement shakes the best solution, or one of several tools?
Step 3: Consult Healthcare Professionals
Seek guidance from:
- Primary care physician
- Geriatric nutritionist or dietitian
- Pharmacist (regarding medication interactions)
- Speech therapist (if swallowing issues exist)
Step 4: Trial Period with Monitoring
If proceeding with meal replacement shakes:
- Start with a 2-4 week trial period
- Monitor weight, energy levels, and overall wellbeing
- Track any digestive issues or side effects
- Assess impact on social eating and quality of life
- Adjust approach based on results
Step 5: Regular Reassessment
Ongoing evaluation should include:
- Monthly weight checks
- Quarterly nutritional status reviews
- Annual comprehensive assessments with healthcare team
- Continuous monitoring of satisfaction and quality of life
Conclusion: Informed Choices for Better Outcomes
The pros and cons of meal replacement shakes for elderly individuals are nuanced and highly personal. These products can be valuable nutritional tools—even lifesaving in certain circumstances—but they’re not universal solutions and come with legitimate drawbacks that deserve consideration.
From my journey with my grandmother and conversations with countless other families, I’ve learned that the best outcomes occur when:
✨ Meal replacement shakes supplement rather than replace whole foods whenever possible
✨ Decisions are made collaboratively with healthcare professionals
✨ Individual preferences, values, and quality of life remain central considerations
✨ Regular monitoring and adjustment occur as needs change
✨ The social and emotional aspects of eating are protected and prioritized
If you’re considering meal replacement shakes for yourself or a loved one, I encourage you to:
Your Next Steps:
- Schedule a consultation with a geriatric nutritionist or registered dietitian
- Conduct a thorough assessment of current nutritional status and eating challenges
- Research appropriate products for specific health conditions and preferences
- Calculate realistic costs and explore financial assistance options if needed
- Start with a trial period rather than committing to long-term use immediately
- Maintain open communication with the elderly person about their preferences and experiences
- Regularly reassess whether the approach is meeting both nutritional and quality-of-life goals
Remember, nutrition in elderly care isn’t just about calories and nutrients—it’s about dignity, pleasure, independence, and connection. The best nutritional strategy honors all these dimensions while meeting medical needs.
Whether meal replacement shakes become a helpful tool in your family’s toolkit or you discover alternative approaches work better, the most important thing is making informed, compassionate decisions that respect the whole person, not just their nutritional requirements.
My grandmother eventually found her balance: one shake for breakfast (when she has little appetite), a social lunch with friends at her retirement community, and a light dinner she prepares herself or shares with family. It’s not perfect, but it works for her—and that’s what matters most.
What works for your family will be unique to your circumstances, but I hope this comprehensive exploration of the pros and cons of meal replacement shakes for elderly individuals helps you make decisions with greater confidence and clarity. 💚
References
[1] Australian Institute of Health and Welfare. (2023). Nutrition and malnutrition in older Australians. AIHW, Australian Government.
[2] Jacobs, D. R., & Tapsell, L. C. (2013). Food synergy: the key to a healthy diet. Proceedings of the Nutrition Society, 72(2), 200-206.
[3] Hooper, L., et al. (2015). Water-loss (intracellular) dehydration assessed using urinary tests: how well do they work? Diagnostic accuracy in older people. American Journal of Clinical Nutrition, 104(1), 121-131.