
I’ll never forget the day my grandmother confessed she’d been eating nothing but toast and tea for weeks. At 82, she’d lost interest in cooking, found grocery shopping exhausting, and didn’t think it mattered much anyway. Within months, she’d lost 15 pounds, her energy had plummeted, and simple tasks became overwhelming. That’s when we discovered the life-changing support of a geriatric nutritionist—a specialist who understood exactly what is a geriatric nutritionist and why an elderly person may need one. Her story isn’t unique, and if you’re reading this, you probably know someone facing similar challenges.
As our loved ones age, their nutritional needs change dramatically, yet this critical aspect of health often gets overlooked. Many families don’t realize that specialized nutrition support exists specifically for older adults, or why it’s so different from general dietary advice. In this comprehensive guide, I’ll walk you through everything you need to know about geriatric nutritionists, the unique challenges facing elderly individuals, and how to determine if this specialized care could make a meaningful difference in your life or the life of someone you love.
Key Takeaways 🔑
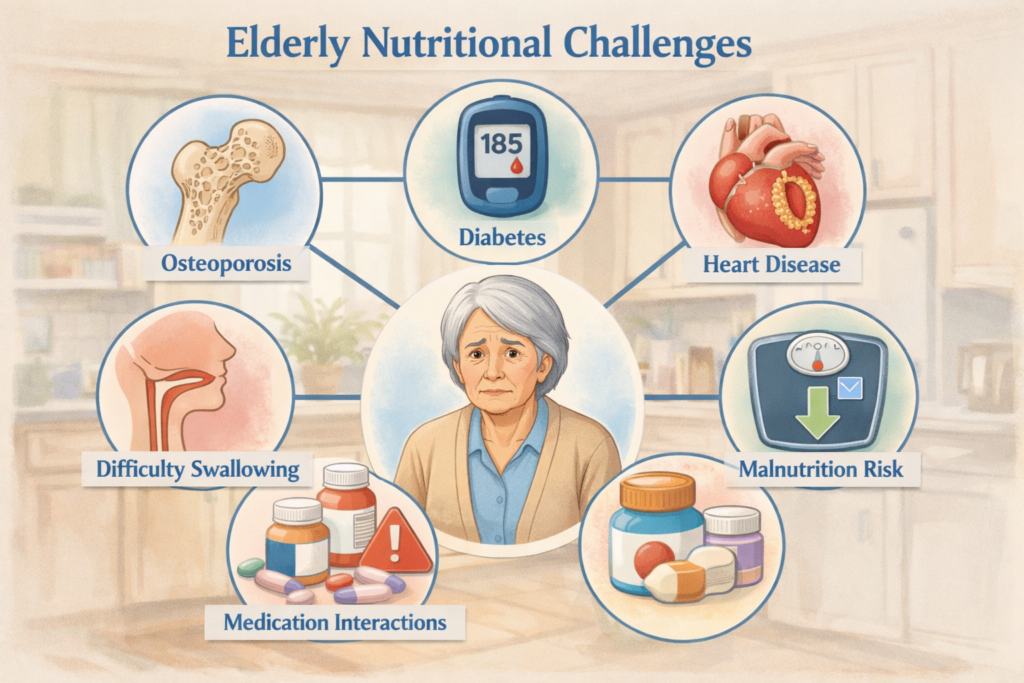
- Geriatric nutritionists are specialized professionals who focus exclusively on the unique nutritional needs, health conditions, and lifestyle factors affecting older adults (typically 65+)
- Elderly individuals face distinct nutritional challenges including decreased appetite, medication interactions, chronic disease management, difficulty chewing or swallowing, and changes in metabolism that require expert guidance
- A geriatric nutritionist can help prevent or manage malnutrition, unintended weight loss, diabetes, heart disease, osteoporosis, and other age-related conditions through personalized nutrition strategies
- Warning signs that indicate the need for a geriatric nutritionist include unexplained weight changes, managing multiple medications, difficulty preparing meals, recent hospitalization, or diagnosis of chronic conditions
- Working with a geriatric nutritionist provides personalized meal plans, practical strategies for real-life challenges, and ongoing support that adapts as needs change over time
Understanding Geriatric Nutritionists: Specialized Experts in Elderly Nutrition

What Exactly Is a Geriatric Nutritionist?
A geriatric nutritionist (also called a geriatric dietitian) is a registered dietitian nutritionist (RDN) who has specialized training and expertise in working with older adults. Unlike general nutritionists who might work with people of all ages, geriatric nutritionists dedicate their practice to understanding the complex interplay between aging, nutrition, chronic diseases, medications, and quality of life in elderly populations.
These professionals typically hold advanced credentials beyond basic nutrition training. Most have completed:
- Bachelor’s and master’s degrees in nutrition, dietetics, or related fields
- Supervised practice through accredited internship programs
- Registration with the Commission on Dietetic Registration (CDR)
- Specialized training in gerontology, geriatric medicine, and aging-related nutrition issues
- Continuing education focused specifically on elderly nutrition research and best practices
The distinction matters tremendously. While any nutritionist can offer dietary advice, geriatric nutritionists understand nuances like how aging affects nutrient absorption, how multiple medications interact with foods, and how to address the psychological and social factors that influence eating habits in older adults.[1]
How Geriatric Nutritionists Differ from General Nutritionists
When my grandmother first started working with her geriatric nutritionist, I was surprised by how different the approach was from the general dietary advice we’d tried before. Here’s what sets geriatric nutritionists apart:
Specialized Knowledge Base:
- Deep understanding of age-related physiological changes (decreased stomach acid, slower metabolism, reduced taste sensitivity)
- Expertise in managing multiple chronic conditions simultaneously
- Knowledge of how 10+ medications might interact with nutrients
- Understanding of age-related conditions like sarcopenia (muscle loss), dysphagia (swallowing difficulties), and cognitive decline
Tailored Assessment Approaches:
- Evaluation of functional abilities (can they shop, cook, open containers?)
- Assessment of social eating situations and isolation factors
- Consideration of fixed incomes and budget constraints
- Screening for depression, grief, and other emotional factors affecting appetite
Practical, Realistic Strategies:
- Meal solutions for those with limited mobility or energy
- Texture modifications for chewing or swallowing difficulties
- Simple recipes that don’t require standing for long periods
- Strategies to make food appealing when taste buds have changed
Credentials and Training to Look For
Not all nutrition professionals have geriatric expertise. When seeking a geriatric nutritionist, look for these credentials:
| Credential | What It Means | Why It Matters |
|---|---|---|
| RDN (Registered Dietitian Nutritionist) | Completed accredited education, supervised practice, and passed national exam | Ensures foundational competency and legal recognition |
| LD or LDN (Licensed Dietitian) | State licensure to practice | Required in most states; provides legal protections |
| CSG (Certified Specialist in Gerontological Nutrition) | Advanced certification in elderly nutrition | Demonstrates specialized expertise in aging populations |
| FAND (Fellow of the Academy) | Highest honor from Academy of Nutrition and Dietetics | Indicates significant contributions to the field |
| Master’s or PhD in Gerontology | Advanced education in aging | Deeper understanding of aging processes |
💡 Pro tip: Always verify credentials through the Commission on Dietetic Registration’s website before working with any nutrition professional.
What Is a Geriatric Nutritionist and Why an Elderly Person May Need One: The Critical Reasons
The Unique Nutritional Challenges of Aging
Aging isn’t just about getting older—it brings profound physiological changes that dramatically affect nutrition. Understanding these changes helps explain what is a geriatric nutritionist and why an elderly person may need one to navigate them successfully.
Physiological Changes That Impact Nutrition
Decreased Appetite and Early Satiety:
As we age, the body produces different levels of hunger hormones. Many older adults experience reduced appetite or feel full after eating very little. This isn’t just being “picky”—it’s a real biological change that can lead to inadequate calorie and nutrient intake.[2]
Changes in Taste and Smell:
By age 70, many people have lost 30-40% of their taste buds. Foods that once seemed flavorful now taste bland, making eating less enjoyable. Salt and sweet tastes are often affected first, leading some elderly individuals to over-salt food or lose interest in eating altogether.
Reduced Digestive Efficiency:
The aging digestive system produces less stomach acid and digestive enzymes, making it harder to break down food and absorb nutrients—particularly vitamin B12, calcium, iron, and protein. This means an elderly person might eat the “right” foods but still develop deficiencies.
Slower Metabolism:
Metabolic rate decreases by about 2% per decade after age 30. Older adults need fewer calories but the same (or more) nutrients, making nutrient density absolutely critical. This narrow window makes every bite count.
Medication Effects:
The average person over 65 takes 4-5 prescription medications daily, and many of these affect nutrition.[3] Some reduce appetite, others deplete specific nutrients, and some interact dangerously with certain foods.
Common Health Conditions Requiring Specialized Nutrition
Geriatric nutritionists are experts in managing the dietary aspects of conditions that predominantly affect older adults:
🫀 Cardiovascular Disease:
Heart disease requires careful management of sodium, saturated fats, and cholesterol while ensuring adequate protein and nutrients. A geriatric nutritionist can create heart-healthy plans that don’t sacrifice taste or cultural food preferences.
🩸 Diabetes:
Managing blood sugar becomes more complex with age, especially when combined with other conditions and medications. Geriatric nutritionists help balance glucose control with preventing malnutrition—a delicate balance many general practitioners miss.
🦴 Osteoporosis:
Bone health requires adequate calcium, vitamin D, protein, and other nutrients, but many medications for osteoporosis affect how the body processes these nutrients. Timing of supplements and foods becomes crucial.
🧠 Cognitive Decline:
Dementia and Alzheimer’s disease create unique nutritional challenges, from forgetting to eat to difficulty using utensils. Geriatric nutritionists develop strategies to maintain nutrition as cognitive abilities change.
💪 Sarcopenia (Muscle Loss):
Age-related muscle loss accelerates after 60, increasing fall risk and reducing independence. Adequate protein intake (often higher than standard recommendations) combined with proper timing is essential but tricky to achieve.[4]
Real-Life Scenarios: When Elderly Individuals Need a Geriatric Nutritionist
Let me share some real stories (names changed) that illustrate what is a geriatric nutritionist and why an elderly person may need one:
Margaret’s Story: The Medication Maze
Margaret, 78, was managing diabetes, high blood pressure, and osteoporosis with seven different medications. She felt constantly nauseous and had lost 20 pounds in six months. Her doctor kept adjusting medications, but nothing helped. A geriatric nutritionist discovered that the timing of her medications and meals was creating the nausea. By restructuring when she ate and took her pills, and adjusting her diet to work with (not against) her medications, Margaret’s nausea resolved and she regained healthy weight.
Robert’s Story: The Widower Who Stopped Cooking
After his wife of 52 years passed away, Robert, 81, essentially stopped eating real meals. He’d never learned to cook and felt overwhelmed by grocery shopping. He survived on frozen dinners, which spiked his blood pressure due to sodium content. A geriatric nutritionist taught him five simple recipes, arranged grocery delivery, and helped him join a senior meal program. His blood pressure normalized, his energy returned, and he told me, “I didn’t realize how bad I felt until I felt good again.”
Linda’s Story: Swallowing Difficulties After Stroke
Linda, 73, developed dysphagia (difficulty swallowing) after a stroke. Regular food was dangerous—she could choke—but the pureed hospital food was so unappetizing she barely ate. A geriatric nutritionist specializing in texture-modified diets created meals that were safe to swallow but actually looked and tasted like real food. Linda went from eating 30% of her meals to 90%, preventing the feeding tube her doctors had recommended.
Warning Signs That Indicate the Need for a Geriatric Nutritionist
How do you know when it’s time to seek specialized nutrition help? Watch for these red flags:
📉 Physical Warning Signs:
- Unintentional weight loss of 5% or more in 3-6 months
- Clothes becoming noticeably loose
- Increased frailty or weakness
- Frequent falls or dizziness
- Slow wound healing
- Frequent infections
- Noticeable muscle wasting
🍽️ Eating-Related Warning Signs:
- Skipping meals regularly
- Eating the same limited foods repeatedly
- Difficulty chewing or swallowing
- Complaints that food “doesn’t taste good anymore”
- Taking more than 45 minutes to eat a meal
- Avoiding social eating situations
- Refrigerator full of expired food
💊 Medical Warning Signs:
- Taking 4+ medications daily
- Recent hospitalization
- New diagnosis of chronic disease
- Poorly controlled diabetes, blood pressure, or cholesterol
- Pressure sores or non-healing wounds
- Constipation or digestive issues
- Laboratory results showing nutrient deficiencies
🧠 Cognitive/Emotional Warning Signs:
- Forgetting to eat or forgetting they’ve already eaten
- Confusion about meal preparation
- Depression or social isolation
- Recent loss of spouse or caregiver
- Difficulty managing grocery shopping or cooking
- Expressing that “it’s too much trouble to eat”
“The most dangerous phrase I hear is ‘I’m just not hungry.’ When elderly individuals lose interest in eating, it’s not a normal part of aging—it’s a red flag that needs professional attention.” — Sarah Chen, RDN, CSG, Geriatric Nutritionist
The Benefits of Working with a Geriatric Nutritionist
Personalized Nutrition Plans for Complex Health Needs
The real value of a geriatric nutritionist lies in their ability to create personalized, practical nutrition plans that address multiple issues simultaneously. This isn’t about generic “eat more vegetables” advice—it’s sophisticated problem-solving.
Comprehensive Assessment Process
When you first meet with a geriatric nutritionist, expect a thorough evaluation that goes far beyond what you eat:
Medical History Review:
- Current diagnoses and health conditions
- Complete medication list (including supplements and over-the-counter drugs)
- Recent laboratory results
- History of surgeries or medical procedures
- Family health history
Functional Assessment:
- Ability to shop for groceries
- Capacity to prepare meals
- Dental health and chewing ability
- Swallowing function
- Hand strength and dexterity (can you open jars, use utensils?)
- Vision and cognitive status
Dietary Assessment:
- Typical daily food intake
- Meal timing and patterns
- Food preferences and cultural considerations
- Appetite and hunger levels
- Digestive symptoms
- Food allergies or intolerances
Lifestyle and Social Factors:
- Living situation (alone, with family, assisted living)
- Financial resources for food
- Transportation access
- Social eating opportunities
- Cultural and religious food practices
- Emotional relationship with food
This comprehensive approach is why geriatric nutritionists can solve problems that stump other healthcare providers. They see the complete picture.
Disease Prevention and Management Through Nutrition
One of the most powerful aspects of geriatric nutrition is its role in preventing and managing chronic diseases. Let me break down how this works:
🔬 Evidence-Based Interventions:
Research consistently shows that proper nutrition can:
- Reduce diabetes medication needs by 30-50% in some cases[5]
- Lower blood pressure as effectively as some medications
- Slow cognitive decline in early dementia
- Reduce fracture risk by improving bone density
- Decrease hospitalization rates by 20-40%
- Improve wound healing time by 50% or more
🎯 Multi-Condition Management:
Here’s where geriatric nutritionists truly shine. Consider someone managing diabetes, kidney disease, and heart disease simultaneously. These conditions have seemingly conflicting dietary requirements:
- Diabetes requires carbohydrate control
- Kidney disease requires protein and potassium restriction
- Heart disease requires sodium limitation
- All three require adequate calories to prevent malnutrition
A geriatric nutritionist can create a plan that addresses all three conditions while ensuring the food is actually enjoyable and sustainable. This sophisticated balancing act is their specialty.
Improving Quality of Life and Independence
Beyond managing diseases, geriatric nutritionists focus on something equally important: helping elderly individuals maintain independence and enjoy life.
Maintaining Functional Independence:
Proper nutrition directly impacts the ability to:
- Live independently at home longer
- Maintain muscle strength for daily activities
- Reduce fall risk
- Preserve cognitive function
- Maintain energy for social activities
- Continue hobbies and interests
Enhancing Social Connection:
Food is deeply social, and geriatric nutritionists understand this. They help elderly individuals:
- Continue enjoying family meals
- Participate in community dining
- Host friends for meals
- Maintain cultural food traditions
- Feel confident eating in public
Preserving Dignity and Autonomy:
A skilled geriatric nutritionist respects that elderly individuals have lived full lives with established preferences. They work with clients, not dictating to them. This collaborative approach preserves dignity while improving health.
Cost-Effectiveness: Preventing Expensive Health Complications
While there’s a cost to working with a geriatric nutritionist, it’s an investment that typically saves money:
Healthcare Cost Reductions:
- Fewer hospitalizations (average cost: $13,000+ per stay)
- Reduced emergency room visits
- Lower medication costs
- Fewer complications from chronic diseases
- Decreased need for nursing home care
Insurance Coverage:
Many insurance plans, including Medicare, cover nutrition counseling for certain conditions:
- Diabetes (10 hours first year, 2 hours annually after)
- Kidney disease
- Post-transplant care
- Cardiovascular disease (in some cases)
Long-Term Savings:
Preventing malnutrition alone saves thousands of dollars. Malnourished elderly individuals have:
- 3x higher hospitalization rates
- 2x longer hospital stays
- 4x higher healthcare costs overall[6]
🏥 Should You See a Geriatric Nutritionist?
Answer these questions to assess whether you or an elderly loved one could benefit from specialized nutrition support
How to Find and Work with a Geriatric Nutritionist
Finding Qualified Geriatric Nutritionists in Your Area
Now that you understand the value of geriatric nutrition support, how do you actually find a qualified professional? Here are proven strategies:
🔍 Professional Directories:
- Academy of Nutrition and Dietetics (eatright.org)
- Use their “Find an Expert” tool
- Filter by specialty: “Gerontological Nutrition”
- Filter by location and insurance accepted
- All listed professionals are verified RDNs
- Commission on Dietetic Registration (cdrnet.org)
- Verify credentials and certifications
- Search for CSG (Certified Specialist in Gerontological Nutrition)
- Check for any disciplinary actions
- Local Hospitals and Medical Centers
- Many have outpatient nutrition services
- Often have geriatric specialists on staff
- May offer group classes as well as individual consultations
💡 Getting Referrals:
- Primary care physicians: Ask for referrals (often required for insurance coverage anyway)
- Geriatricians: Specialists in elderly care usually have nutrition professionals they work with
- Senior centers: Often have relationships with local geriatric nutritionists
- Home health agencies: May have nutritionists on staff or can recommend professionals
- Online communities: Local Facebook groups for seniors or caregivers can provide recommendations
Questions to Ask When Choosing:
When you’ve identified potential geriatric nutritionists, ask these questions before committing:
- “What percentage of your practice focuses on elderly clients?”
- “Do you have specialized training or certification in geriatric nutrition?”
- “Have you worked with clients managing [specific conditions]?”
- “What does a typical first appointment involve?”
- “How often would we meet, and what does ongoing support look like?”
- “Do you provide meal plans, recipes, and practical resources?”
- “Can you coordinate with my other healthcare providers?”
- “What are your fees, and do you accept my insurance?”
What to Expect During Your First Consultation
Understanding what happens during that first appointment can ease anxiety and help you prepare. Here’s what typically occurs:
Before the Appointment:
You’ll likely receive intake forms asking about:
- Medical history and current conditions
- Complete medication list (bring bottles if possible)
- Typical eating patterns
- Lifestyle and living situation
- Goals and concerns
Pro tip: Bring recent lab work, especially if it shows nutrient deficiencies, blood sugar levels, cholesterol, kidney function, or bone density results.
During the Appointment (Usually 60-90 Minutes):
Phase 1: Getting to Know You (20-30 minutes)
The nutritionist will review your health history and ask detailed questions about your eating habits, preferences, challenges, and goals. This isn’t interrogation—it’s collaborative problem-solving.
Phase 2: Assessment (15-20 minutes)
Depending on the setting, this might include:
- Weight and height measurements
- Body composition analysis
- Review of food diary (if you kept one)
- Discussion of laboratory results
- Functional assessment (grip strength, chewing ability, etc.)
Phase 3: Education and Goal-Setting (20-30 minutes)
The nutritionist will:
- Explain how your conditions relate to nutrition
- Identify priority areas for intervention
- Discuss realistic, achievable goals
- Begin outlining strategies tailored to your situation
Phase 4: Action Plan (10-15 minutes)
You’ll leave with:
- Initial recommendations to implement
- Resources (recipes, shopping lists, meal ideas)
- Schedule for follow-up appointments
- Clear next steps
After the Appointment:
Within a week, you’ll typically receive:
- Written summary of your consultation
- Personalized meal plan or eating guidelines
- Educational materials
- Contact information for questions
Insurance Coverage and Cost Considerations
One of the biggest questions I hear is: “Can I afford this?” Let’s break down the financial aspects:
💰 Medicare Coverage (2026):
Medicare Part B covers Medical Nutrition Therapy (MNT) for:
- Diabetes: 10 hours of counseling in the first year, then 2 hours annually
- Kidney disease: Same coverage as diabetes
- Post-kidney transplant: Coverage for 36 months
Requirements:
- Must be provided by a registered dietitian
- Requires physician referral
- No copay if provider accepts Medicare assignment
🏥 Private Insurance:
Coverage varies widely, but many plans cover nutrition counseling for:
- Diabetes management
- Cardiovascular disease
- Obesity (BMI over 30)
- Eating disorders
- Pregnancy-related conditions
Check your specific plan:
- Call the number on your insurance card
- Ask: “Do you cover nutrition counseling with a registered dietitian?”
- Ask: “What conditions qualify for coverage?”
- Ask: “How many sessions per year are covered?”
- Ask: “Do I need a referral from my doctor?”
💵 Out-of-Pocket Costs:
If you’re paying privately, expect:
- Initial consultation: $150-$300 (60-90 minutes)
- Follow-up sessions: $75-$150 (30-45 minutes)
- Package deals: Some nutritionists offer 3-6 session packages at reduced rates
Ways to Reduce Costs:
- Use HSA/FSA funds: Nutrition counseling qualifies for tax-advantaged health savings accounts
- Ask about sliding scale fees: Some practitioners offer reduced rates based on income
- Group classes: Often more affordable than individual sessions
- Senior center programs: Many offer free or low-cost nutrition services
- Telehealth options: Virtual appointments may cost less than in-person visits
Is It Worth the Investment?
Consider this perspective: One hospitalization prevented pays for years of nutrition counseling. One medication reduced or eliminated saves hundreds monthly. The independence maintained is priceless.
Telehealth Options for Geriatric Nutrition Services
The rise of telehealth has made geriatric nutrition services more accessible than ever, especially for those with mobility challenges or living in rural areas.
✅ Advantages of Virtual Consultations:
- No transportation needed (huge for those who no longer drive)
- Appointments from the comfort of home
- Family members in different locations can join
- Easier to show your actual kitchen, food, and eating environment
- Often more scheduling flexibility
- Sometimes lower cost than in-person visits
📱 What You’ll Need:
- Computer, tablet, or smartphone with camera and microphone
- Reliable internet connection
- Email address for receiving documents
- Ability to weigh yourself at home (or family member to help)
Popular Telehealth Platforms for Geriatric Nutrition:
Many geriatric nutritionists now offer virtual services through:
- Zoom, Doxy.me, or other HIPAA-compliant video platforms
- Specialized nutrition platforms like NutriAdmin or Practice Better
- Hospital system patient portals
Insurance Coverage for Telehealth:
Since the COVID-19 pandemic, most insurance plans (including Medicare) now cover telehealth nutrition counseling at the same rate as in-person visits. However, verify with your specific plan.
Making the Most of Your Geriatric Nutrition Journey
Preparing for Your Appointments
To get maximum value from your time with a geriatric nutritionist, come prepared:
📋 Documents to Bring:
- Complete medication list (prescriptions, over-the-counter, supplements)
- Recent laboratory results
- List of healthcare providers and their contact information
- Food diary (3-7 days if possible)
- List of questions and concerns
📝 Keeping a Helpful Food Diary:
If your nutritionist asks you to track your eating, include:
- Everything you eat and drink (including water)
- Approximate portions (use household measures: “1 cup,” “palm-sized”)
- Times of meals and snacks
- Where you ate and with whom
- How you felt (hungry, satisfied, too full, nauseous)
- Any symptoms (bloating, heartburn, fatigue)
Don’t try to eat “perfectly” during the tracking period—your nutritionist needs to see your real patterns, not an idealized version.
Setting Realistic Goals and Expectations
One of the most important aspects of working with a geriatric nutritionist is setting achievable goals. Here’s what realistic looks like:
🎯 Good Goals:
- “I want to stop losing weight and maintain my current weight”
- “I’d like to reduce my diabetes medication by improving my diet”
- “I want to have more energy to play with my grandchildren”
- “I’d like to prepare at least one healthy meal per day”
❌ Unrealistic Goals:
- “I want to reverse 20 years of osteoporosis in 3 months”
- “I’ll completely change my eating habits overnight”
- “I’ll never eat my favorite foods again”
- “I’ll follow a perfect diet 100% of the time”
Timeline Expectations:
- Immediate (1-2 weeks): Small habit changes, reduced symptoms like heartburn or constipation
- Short-term (1-3 months): Improved energy, better blood sugar control, modest weight changes
- Medium-term (3-6 months): Measurable improvements in lab values, medication adjustments
- Long-term (6+ months): Sustained health improvements, new habits firmly established
Involving Family Members and Caregivers
Geriatric nutrition is rarely a solo endeavor. Family involvement often makes the difference between success and struggle.
👨👩👧👦 How Family Can Help:
- Attend appointments: Extra ears hear information you might miss
- Share meal preparation: Make healthy eating a family activity
- Provide transportation: To grocery stores, appointments, senior meal programs
- Offer encouragement: Celebrate small victories and progress
- Help with implementation: Meal prep, grocery shopping, cooking assistance
For Long-Distance Caregivers:
If you’re supporting an elderly parent from afar:
- Request permission to join telehealth appointments
- Set up grocery delivery services
- Arrange meal delivery programs
- Schedule regular check-in calls around mealtimes
- Coordinate with local family or friends for hands-on support
Communication Tips:
When discussing nutrition with elderly loved ones:
- Focus on abilities, not limitations
- Emphasize what they can eat, not restrictions
- Respect their autonomy and preferences
- Avoid being the “food police”
- Celebrate improvements, no matter how small
Tracking Progress and Celebrating Wins
Monitoring progress helps maintain motivation and allows your nutritionist to adjust strategies as needed.
📊 Metrics to Track:
Beyond the scale, consider tracking:
- Energy levels: Rate 1-10 daily
- Appetite: Note improvements or concerns
- Meal completion: Are you finishing meals?
- Symptom changes: Reduced heartburn, better digestion, less fatigue
- Functional improvements: Walking farther, standing longer, better balance
- Medication changes: Reduced doses or discontinued medications
- Lab value improvements: Blood sugar, cholesterol, vitamin levels
- Quality of life: Social eating, cooking confidence, independence
🎉 Celebrating Non-Scale Victories:
Some of the most meaningful wins have nothing to do with weight:
- “I cooked a meal for the first time in months”
- “I had enough energy to attend my grandson’s soccer game”
- “My doctor reduced my diabetes medication”
- “I enjoyed eating again”
- “I felt confident eating at a restaurant with friends”
- “I’m sleeping better”
- “My constipation resolved”
These victories deserve celebration! Share them with your nutritionist, family, and friends.
Common Myths and Misconceptions About Geriatric Nutrition
Let’s address some widespread misunderstandings that prevent elderly individuals from getting the nutrition support they need:
❌ Myth #1: “Weight loss is normal and healthy as you age.”
✅ Reality: While some weight change occurs with aging, significant unintentional weight loss is never normal and indicates a problem requiring attention. It’s associated with increased mortality, hospitalization, and functional decline.[7]
❌ Myth #2: “Elderly people need fewer nutrients.”
✅ Reality: Older adults need the same or more of most nutrients (especially protein, calcium, vitamin D, and B12) but fewer calories. This makes nutrient density absolutely critical.
❌ Myth #3: “It’s too late to improve health through nutrition changes.”
✅ Reality: Research consistently shows that nutrition interventions benefit people at any age. I’ve seen 90-year-olds improve their health, energy, and independence through dietary changes.
❌ Myth #4: “Geriatric nutritionists just tell you to eat less.”
✅ Reality: Geriatric nutritionists often encourage eating more—more protein, more nutrient-dense foods, more frequent meals. Restriction is rarely the goal.
❌ Myth #5: “If my doctor hasn’t mentioned nutrition, it must not be important.”
✅ Reality: Most physicians receive minimal nutrition training (average of 19 hours throughout medical school). They may not recognize nutrition issues or know when to refer to specialists.
❌ Myth #6: “Nutrition counseling means giving up all my favorite foods.”
✅ Reality: Good geriatric nutritionists work with your preferences and cultural traditions, finding ways to include foods you love while improving overall nutrition.
❌ Myth #7: “I’ve eaten this way my whole life; I can’t change now.”
✅ Reality: While habits are strong, small, gradual changes are absolutely achievable at any age. Geriatric nutritionists specialize in realistic, sustainable modifications.
Frequently Asked Questions About Geriatric Nutritionists

Q: What’s the difference between a nutritionist and a dietitian?
A: The term “nutritionist” isn’t regulated in most states—anyone can call themselves a nutritionist. “Registered Dietitian Nutritionist” (RDN) is a protected credential requiring specific education, supervised practice, and passing a national exam. Always look for the RDN credential.
Q: How long will I need to work with a geriatric nutritionist?
A: It varies. Some people need just a few sessions to get on track, while others benefit from ongoing support. Typical patterns include intensive support for 2-3 months, then periodic check-ins (monthly or quarterly) for maintenance and adjustments.
Q: Can a geriatric nutritionist help if I have dementia?
A: Absolutely. Geriatric nutritionists have strategies for maintaining nutrition as cognitive abilities change, including working with caregivers, simplifying meal routines, and addressing eating challenges common in dementia.
Q: Will I have to cook complicated recipes?
A: No! Geriatric nutritionists specialize in simple, practical solutions. They understand that many elderly individuals have limited energy, mobility, or cooking skills. Recommendations are always tailored to your abilities.
Q: What if I live in a nursing home or assisted living facility?
A: Geriatric nutritionists can still help by reviewing facility menus, making recommendations for meal choices, suggesting supplements if needed, and advocating for your nutritional needs with facility staff.
Q: Can a geriatric nutritionist help with tube feeding?
A: Yes. Many geriatric nutritionists have expertise in enteral nutrition (tube feeding), including formula selection, administration schedules, and transitioning back to oral eating when possible.
Q: How is geriatric nutrition different from pediatric nutrition?
A: While both are specialized fields, they address opposite ends of the life spectrum. Pediatric nutrition focuses on growth and development, while geriatric nutrition focuses on maintaining function, managing chronic diseases, and preventing decline. The physiological considerations, common conditions, and intervention strategies are completely different.
Taking Action: Your Next Steps
If you’ve read this far, you’re clearly invested in understanding how geriatric nutrition can help. Now it’s time to take action.
Immediate Actions You Can Take Today
If you’re concerned about yourself:
- Complete the assessment tool earlier in this article to gauge your need
- Schedule your annual wellness visit and discuss nutrition concerns with your doctor
- Start a simple food diary for 3-7 days to identify patterns
- Research geriatric nutritionists in your area using the resources mentioned
- Check your insurance coverage for nutrition counseling
If you’re concerned about an elderly loved one:
- Have a gentle conversation about nutrition concerns you’ve noticed
- Offer to attend their next doctor’s appointment to discuss nutrition
- Use the assessment tool together to objectively evaluate needs
- Research local resources including senior meal programs and nutrition services
- Offer specific help: “Can I take you to a nutrition appointment?” rather than vague “Let me know if you need anything”
Resources for Continued Learning
Professional Organizations:
- Academy of Nutrition and Dietetics (eatright.org) – Consumer nutrition information
- American Society for Nutrition (nutrition.org) – Research and science-based information
- National Institute on Aging (nia.nih.gov) – Aging and health resources
Books on Geriatric Nutrition:
- “Nutrition and Aging” by Melissa Bernstein and Kimberley McManus
- “The Complete Guide to Nutrition in Primary Care” – includes geriatric sections
- “Meals on Wheels: The Ultimate Guide to Nutrition and Aging”
Meal Delivery and Support Services:
- Meals on Wheels America (mealsonwheelsamerica.org) – Find local programs
- Mom’s Meals (momsmeals.com) – Medically tailored meal delivery
- Silver Cuisine (silvercuisine.com) – Senior-focused meal delivery
Online Communities:
- Caregiver Action Network forums
- AARP online community
- AgingCare.com forums
Building Your Support Team
Remember, a geriatric nutritionist is part of a larger healthcare team. Your ideal support system includes:
- Primary care physician: Coordinates overall care
- Geriatrician: Specializes in elderly health
- Geriatric nutritionist: Addresses nutrition needs
- Pharmacist: Monitors medication interactions
- Physical therapist: Maintains mobility and strength
- Social worker: Connects to community resources
- Family and friends: Provides daily support and encouragement
Each professional brings unique expertise, and they work best when communicating with each other. Don’t hesitate to request that your geriatric nutritionist coordinate with your other providers.
Conclusion: Investing in Nutritional Health for Better Aging
As I reflect on my grandmother’s journey with geriatric nutrition support, I’m filled with gratitude for the difference it made. She didn’t just regain the weight she’d lost—she regained her energy, her independence, and her joy in eating. She lived four more vibrant years, hosting family dinners, traveling to visit grandchildren, and maintaining her own home. That’s the power of specialized geriatric nutrition care.
Understanding what is a geriatric nutritionist and why an elderly person may need one isn’t just academic knowledge—it’s potentially life-changing information. The aging process brings unique nutritional challenges that deserve specialized expertise. From managing multiple chronic conditions to navigating medication interactions, from addressing swallowing difficulties to maintaining muscle mass, geriatric nutritionists possess the knowledge and skills to help elderly individuals thrive, not just survive.
The warning signs are clear: unintentional weight loss, multiple medications, chronic health conditions, difficulty eating or preparing meals, recent hospitalization, or declining energy and function. If any of these resonate with your situation or that of someone you love, don’t wait. Nutrition issues rarely improve on their own and often worsen over time.
The investment in geriatric nutrition services—whether covered by insurance or paid out-of-pocket—pays dividends in improved health, maintained independence, reduced hospitalizations, and enhanced quality of life. It’s not about adding years to life; it’s about adding life to years.
Your action plan starts now:
✅ Use the assessment tool in this article to evaluate needs objectively
✅ Schedule a conversation with your healthcare provider about nutrition concerns
✅ Research qualified geriatric nutritionists in your area
✅ Check insurance coverage and financial options
✅ Take the first step—make that phone call, schedule that appointment, start that conversation
Remember, seeking help isn’t a sign of weakness or failure—it’s a sign of wisdom and self-care. Every elderly individual deserves to eat well, feel well, and live well. A geriatric nutritionist can be the key to making that happen.
The question isn’t whether you can afford to work with a geriatric nutritionist. The real question is: can you afford not to?
References
[1] Bernstein, M., & Munoz, N. (2022). Nutrition for the Older Adult (3rd ed.). Jones & Bartlett Learning.
[2] Landi, F., et al. (2016). “Anorexia of aging: risk factors, consequences, and potential treatments.” Nutrients, 8(2), 69.
[3] Maher, R. L., Hanlon, J., & Hajjar, E. R. (2014). “Clinical consequences of polypharmacy in elderly.” Expert Opinion on Drug Safety, 13(1), 57-65.
[4] Cruz-Jentoft, A. J., et al. (2019). “Sarcopenia: revised European consensus on definition and diagnosis.” Age and Ageing, 48(1), 16-31.
[5] American Diabetes Association. (2023). “Standards of Medical Care in Diabetes—2023.” Diabetes Care, 46(Supplement_1).
[6] Kaiser, M. J., et al. (2010). “Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment.” Journal of the American Geriatrics Society, 58(9), 1734-1738.
[7] Morley, J. E. (2017). “Weight loss in older persons: new therapeutic approaches.” Current Pharmaceutical Design, 23(28), 4073-4075.